
Back pain is an issue that affects people of all ages and lifestyles. Whether its caused by poor posture, muscle strain, lack of exercise or certain underlying conditions, finding relief is essential for maintaining mobility and overall well-being.
When experiencing back pain, the instinct may be to rest and avoid movement. However, in many cases, staying sedentary can make the symptoms worse and lead to further discomfort. Movement on the other hand promotes blood flow, strengthens muscles and improves flexibility, all of which works great for supporting the spine and reducing pain.
Therefore, it’s essential to prioritize movement and activity in everyday life. Simple changes such as taking frequent breaks from sitting, practicing good posture and incorporating gentle movements throughout the day can make a significant difference in managing back pain and promoting spinal health.
Regular exercise is one of the most effective ways to manage back pain and prevent future episodes. Low-impact exercises such as walking, swimming and cycling can help strengthen the muscles in the back and core, providing stability and support for the spine. However, remember to start slowly and gradually increase the intensity and duration of your workouts to avoid overexertion and injury.
Yoga offers back pain management by combining physical postures, breathing techniques and meditation to promote healing and relaxation. Specific yoga poses such as cat-cow stretch, child’s pose, superman stretch and downward-facing dog, target the muscles along the spine helping to release tension and discomfort.
Physical therapy is a tailored approach to back pain management, guided by a trained professional who can assess individual needs and develop a personalized treatment plan. Through targeted exercises, manual techniques and therapeutic modalities, physical therapists address muscle imbalances and improve posture. Moreover, they provide education on injury prevention and self-management strategies to empower patients on their journey to recovery.
Back pain can be a challenging condition but with the right approach, relief is possible. By embracing movement through exercise, yoga and physical therapy, individuals can strengthen their bodies and find relief from discomfort. Whether it’s a gentle walk or a yoga session, taking proactive steps towards movement and mobility is key to living a life free from back pain.

Spondylitis is a term used to describe inflammation of the vertebrae in the spine, which can lead to chronic pain and discomfort. This condition can affect people of all ages and is often associated with conditions such as ankylosing spondylitis and cervical spondylitis. Let’s take a look at what causes spondylitis and how it can be treated.
The symptoms of spondylitis can manifest differently based on the type and severity of the condition. Typical symptoms include chronic back or neck pain accompanied by stiffness in the spine, pain and inflammation in the hips, shoulders and other joints, feelings of fatigue and discomfort particularly after prolonged periods of inactivity, radiating pain or numbness in the arms or legs, etc. In severe cases of cervical spondylitis, individuals may encounter difficulty breathing or swallowing as well due to compression of the spinal cord.
Spondylitis can stem from various underlying causes which may include genetics, autoimmune disorders, trauma or injury to the spine and infections. Genetic factors like ankylosing spondylitis often run in families. Autoimmune disorders such as rheumatoid arthritis and psoriatic arthritis can provoke inflammation in the spine, also contributing to spondylitis. Traumatic incidents or injuries affecting the spine can also trigger inflammation and damage leading to spondylitis. Additionally, bacterial or viral infections targeting the spine can result in inflammation and the onset of spondylitis.
The management of spondylitis typically involves a multifaceted approach comprising lifestyle adjustments and medication. Common treatment modalities include physical therapy which employs targeted exercises and stretches to enhance flexibility and strengthen spinal muscles that helps to relieve pain and shooting stiffness. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), painkillers and muscle relaxants may be prescribed to reduce inflammation and discomfort. Heat and cold therapy can offer temporary relief from symptoms by applying heat packs or ice packs to the affected area. Lifestyle modifications such as maintaining a healthy weight and posture are essential for managing spondylitis and preventing flare-ups. In severe cases where conservative treatments prove ineffective, surgical interventions like spinal fusion or decompression surgery may be considered to stabilize the spine and alleviate pressure on affected nerves.
Spondylitis is a complex condition that requires a multidisciplinary approach to management. By understanding the symptoms, causes and treatment options for spondylitis, individuals can take proactive steps to relieve pain and enhance their overall quality of life.

Back tension often leads to stress and poor posture can wreak havoc on our bodies and minds. Fortunately, there are numerous ways to alleviate this discomfort and promote relaxation. Incorporating techniques like stretching, meditation, heat therapy and chiropractic care can help ease muscle tension and enhance overall well-being.
Stretching is very powerful in the battle against back tension. By gently elongating the muscles along your spine, you can relieve stiffness and promote flexibility. Incorporate stretches like the cat-cow stretch and spinal twist to release tension and improve mobility. Regular stretching sessions can work wonders in loosening tight muscles and promoting relaxation throughout your body.
Stress often manifests as tension in our muscles including those in the back. Combat this stress with breathing that focuses on deep, intentional breaths. Practice diaphragmatic breathing, inhaling deeply through your nose and exhaling slowly through your mouth. This approach can calm your nervous system and reduce muscle tension.
Heat compress is a great method for relaxing tense muscles and soothing discomfort. Apply a heating pad or warm compress to your back for gentle warmth and relief. The heat helps increase blood flow to the area and promotes relaxation while relieving muscle tension. By incorporating heat therapy into your self-care routine, you can melt away stress and tension from your muscles.
Chiropractic adjustments offer targeted relief for back tension by realigning the spine and restoring proper function to the nervous system. A skilled chiropractor can identify areas of misalignment and apply gentle adjustments to alleviate pressure on the nerves and muscles. Regular chiropractic visits can help address underlying issues contributing to back tension and promote long-term musculoskeletal health.
By incorporating these strategies into your daily routine, you can effectively manage back tension and promote overall muscle relaxation. Whether it’s through stretching, deep breathing, heat compress or chiropractic care, taking proactive steps to look after your muscles and soothe your stress can lead to improved physical and emotional well-being. Say farewell to back tension and hello to a healthier and happier you.

The post cancer journey is an incredibly challenging time for patients and their families as they navigate the complexities of terminal illness. In this stage, the focus shifts from curing the disease to providing comfort and enhancing the quality of life. GINONCO, a nutraceutical product enriched with ginseng that holds the potential to offer support and relief for individuals on this difficult path, along with Picrorhiza kurroa extract and Silybum marianum extract that further provides comfort and eases physical and emotional distress. In this blog, we explore how GINONCO can play a crucial role in enhancing the well-being of patients facing this challenging phase.
For patients in this stage, pain, fatigue and discomfort can become constant companions. As the focus shifts to palliative care, the primary goal is to alleviate suffering and enhance the quality of remaining life. Emotional distress, anxiety and feelings of helplessness can also be overwhelming for both patients and their loved ones during this time.
GINONCO proves highly effective in reducing the occurrence of nausea and vomiting induced by various cancer treatments including chemotherapy drugs, radiation therapy, immunotherapy, and surgery. Its remarkable ability to alleviate these distressing side effects provides patients with much-needed relief and comfort during their treatment journey. Furthermore, it goes beyond just symptom management. It plays a vital role in boosting physical stamina and combating the fatigue often associated with cancer. By enhancing energy levels, it also empowers patients to regain strength and endurance allowing them to engage in daily activities with renewed vigor.
The potent combination of antioxidants and anti-inflammatory properties found in GINONCO provides robust support in reducing oxidative stress and inflammation commonly observed during cancer treatments. This protective effect aids in preserving healthy tissues and minimizing potential damage caused by cancer therapies. Additionally, its remarkable immune-strengthening properties play a pivotal role in supporting patients during their cancer treatment. It also helps patients maintain optimal immune function, increasing their resilience against infections and other complications.
More than just a physical aid, GINONCO also contributes to an improved sense of well-being. Its positive impact on patients’ overall health and vitality empowers them to navigate their recovery journey with a renewed sense of positivity and optimism. Embracing it as part of a comprehensive cancer care plan ensures patients receive holistic support during their treatment. With its multifaceted benefits, GINONCO becomes a valuable ally in the fight against cancer, helping patients not only endure the challenges of treatment but also thrive with newfound strength and vitality.

Chemotherapy, often referred to simply as “chemo” is a powerful and widely recognized treatment for cancer. For many individuals diagnosed with cancer like breast cancer, oral cancer, blood cancer, etc, the word “chemotherapy” can evoke a sense of fear and uncertainty. However, understanding the fundamentals of chemotherapy can demystify this critical aspect of cancer care. In this blog, we delve into the world of chemotherapy, shedding light on how it works and its role in cancer treatment.
Chemotherapy is a medical treatment that uses powerful drugs to target and kill rapidly dividing cells in the body. It is commonly used to treat cancer, which is characterized by the uncontrolled growth and division of abnormal cells. The main goal of chemotherapy is to stop or slow down the growth of cancer cells, reduce the size of tumors, and ultimately, improve the patient’s quality of life and increase their chances of survival.
Chemotherapy encompasses a diverse array of drugs, each with unique mechanisms of action and applications. The type of chemotherapy prescribed depends on the specific cancer type, its stage, and the patient’s overall health.
While chemotherapy primarily targets cancer cells, it can also affect healthy cells that divide rapidly, such as those in the bone marrow, gastrointestinal tract, and hair follicles. This accounts for some of the side effects associated with this treatment. Common side effects may include hair loss, fatigue, nausea, vomiting, and a decreased ability to fight infections.
Chemotherapy, while effective in treating cancer, can have a profound impact on a patient’s quality of life due to its side effects. However, several emerging trends, including the use of nutraceuticals, offer relief from these adverse effects. Natural ingredients like Korean red ginseng and zinziber officinale have shown promise in supporting recovery after chemotherapy by boosting the immune system. Numerous products in the market boast these ingredients, but GINONCO by Immunity Bloom stands out for offering the purest forms, providing relief from various types of treatments for cancers like breast cancer, oral cancer, and blood cancer. As we continue our fight against cancer, it becomes crucial to acknowledge the importance of both chemotherapy and supportive therapy in alleviating the burden of cancer treatment on patients.

Cancer is a global health burden affecting millions of lives worldwide. Its prevalence is rising steadily over the years with no discrimination between genders, age groups or geographical locations. Cancer is responsible for millions of new cases and deaths annually. Cancer often lurks in the shadows during its early stages, evading detection and quietly spreading its roots. Sadly, the initial stage of cancer goes unnoticed or absent altogether and the lack of recognizable warning signs can lead individuals to overlook or dismiss the severity of the situation. This leads to delaying of critical medical attention and as time passes, the undiagnosed cancer can grow and spread to the surrounding healthy tissues, reducing the chances of a full recovery. Cancer can happen to anyone and early detection remains our most potent weapon in the battle against cancer. In this blog, we are going to be discussing ways in which you can potentially detect some types of cancers early and save yourself from future complications.
Breast cancer is a cancer that forms in the cells of the breast. It is quite popular to check your breast for lumps frequently as it is a clear symptom of breast cancer. Other symptoms include bloody discharge from nipple, changes in shape or texture of nipple or breast, etc. However, there is a method to diagnose breast cancer even before the lump is visible called Mammography. Mammography is the process of using low energy X-rays to examine the human breast for early detection of cancer and other breast diseases. A yearly mammography is advised to women of age 40+ to detect whether there is anything to worry about.
Oral cancer is the cancer that develops in any part of the mouth. It is quite easy to detect by looking out for any lesions, patches or wounds in the mouth. Dentists and oral health professionals are trained to recognize suspicious lesions or abnormalities in the mouth, tongue, lips, gums, and throat so getting a routine dental checkup will not just help to keep your oral hygiene at its peak but will also alert you of potential early cancer in the early stage as well.
Lung cancer is a cancer that begins in the lungs and most often occurs in people who smoke. Knowing the early symptoms of lung cancer can prompt early medical evaluation. Common symptoms include persistent cough, chest pain, shortness of breath, unexplained weight loss, and recurrent respiratory infections. Regular health check-ups are very important in early detection and if lung cancer is suspected, additional diagnostic tests such as chest X-rays, CT scans, sputum cytology, bronchoscopy or biopsy can help confirm the presence of cancer and determine its stage and extent.
Stomach cancer is a cancer that starts in the cells lining the stomach. Symptoms include feeling bloated after eating, feeling full after eating small amounts of food, nausea, heartburn or indigestion. Endoscopy is a vital tool for detecting stomach cancer in its early stages. An endoscopy is a procedure in which a thin, flexible tube with a camera on the end is inserted into the esophagus and stomach. It allows doctors to visually examine the stomach lining and take biopsies if any abnormal areas are found.
Menopause is an event that occurs in every women’s life once they turn a certain age. As we all know, the estrogen levels in the body starts declining resulting in the cessation of periods and fertility. But is this declining estrogen anyway related to your bone health? Does the occurrence of menopause lead to weakness in your bones or muscle fatigue? The answer is yes, menopause and bone health infact are interlinked to one another and that’s why you need to take appropriate measures to make sure that your bones stay strong even after menopause.
The estrogen in your body helps to enhance the absorption of calcium from your intestines which contributes in strengthening bones as well as helps to prevent excessive bone loss. It provides like a balance between bone formation and bone breakdown which helps us maintain optimal bone density. However, during menopause, when estrogen levels decline, this effect also diminishes leading to an increased risk of bone loss that causes consistent joint pain. As bone loss makes your bones really fragile, you become more susceptible to osteoporosis and bone fractures.
Not just your bones, but estrogen also helps in maintaining muscle mass by promoting protein synthesis. It helps in muscle contraction that gives you extra strength during activities that require muscle exertion. It also boosts energy production within muscle cells however, a decline in estrogen levels will lead to a decrease in the energy production, a gradual loss of muscle mass and a decrease in muscle strength, which will lead to increased muscle fatigue.
Make sure that you are consuming enough calcium daily. It could either be through your diet like consuming dairy products and green leafy vegetables, or you can also take calcium supplements. Vitamin D is very important for the absorption of calcium so make sure you are getting proper sun exposure. Nutraceuticals can offer great combination of important nutrients required for everyday nutritional meets as well as help to target specific concerns like joint pain. Regular exercise on the other hand, can help you build and maintain muscle mass.

Menopause is a natural transition that occurs in every woman’s life and hormones play a significant role in it. Hormones contribute to various things right from the changes that are occurring in your body to how you feel during those changes. The major hormones that drive the menopausal transition are Estrogen, Progesterone and FSH as well as Cortisol and Norepinephrine that further contribute to the menopausal symptoms. During the menopause journey, your estrogen and progesterone declines gradually while FSH levels increase.
Estrogen is one of the key hormones in the female reproductive system, responsible for regulating the menstrual cycle. It also helps in supporting the health of the reproductive organs and maintaining bone density. During menopause, the ovaries gradually decrease their production of this hormone. This decline in estrogen leads to various physical and emotional changes associated with menopause like hot flashes, vaginal dryness, mood swings and changes in bone density.
Progesterone is another hormone produced by the ovaries to prepare the uterus for pregnancy. During menopause, progesterone production declines along with estrogen. It is due to the decline of this hormone that marks the inability of a woman to get pregnant anymore. Estrogen and Progesterone both have antioxidant properties which in turn helps to reduce the oxidative stress in the body. Due to the declining hormones, it can impact oxidative stress levels like changes in cellular functioning including mitochondrial functioning or impact on cardiovascular health, bone density and cognitive function.
FSH plays a role in stimulating the growth and maturation of ovarian follicles, which contain the eggs. As estrogen levels decrease, the body tries to make up for it and there is an increase in the FSH levels as the body attempts to stimulate the ovaries to produce estrogen. This increased FSH can affect libido (sex drive) in women.
During menopause, women experience extra stress due to dysregulation of the body’s stress response system. This means more than increased levels of the stress hormones like Cortisol and Norepinephrine. Elevated cortisol levels exacerbate menopausal symptoms such as mood swings and sleep disturbances. It may also contribute to the onset or worsening of conditions like anxiety and depression during menopause. Norepinephrine on the other hand regulates temperature in the body and alterations in its levels contribute to frequent occurrence of sudden hot flashes.

Menopause brings about a multitude of changes in a woman’s body and one very common symptom is the increased susceptibility of contracting UTI that is, Urinary Tract Infections. This happens because during menopause, levels of estrogen in your body decline, causing alterations in the pH level in your urinary tract. This dropped pH level becomes a hub for harmful bacteria like E.Coli increasing the likelihood of developing UTIs. UTIs cause a great deal of discomfort in day to day life along with associated symptoms such as a need to urinate more often than usual, a burning sensation while peeing, pelvic pain and more. This pain and discomfort, if not managed, may result in persistent irritation. To manage this and provide relief from menopausal UTIs, D-Mannose has gained popularity as a natural remedy.
D-Mannose is a simple sugar molecule. When consumed orally, it gets absorbed into the bloodstream and then goes via the kidneys into the urine. In the urinary tract, D-Mannose attaches itself to the bacteria present there (mostly E.Coli), coats it and prevents it from getting attached to the walls of the urinary tract. Due to this detachment from the urinary tract walls, the bacteria gets flushed out of the body when you pee, thus reducing its ability to stay and cause infection.
D-Mannose is not just used by menopausal women, but also by anyone who is looking at natural alternatives for managing UTI. It is not just used as a treatment option, but can be also used by those who want to prevent the occurrence of UTI. This includes people who are prone to urinary tract infections and experience recurrent UTIs.
Good for you! There is a product on the market that not only assists with menopausal UTI, but also helps in managing other symptoms of menopause as well such as hot flashes, night sweats, mood swings, hormonal imbalance and more. This product – MENOBLOOM, uses high quality ingredients to support women through their menopausal journey. Now you don’t have to worry about various symptoms of menopause individually when you can just manage all of them with a single capsule a day.

Menopause marks the end of a woman’s menstrual cycles and fertility. It involves several hormonal changes and menopausal symptoms at different stages of menopause. Let’s understand what actually happens during the various stages of menopause. The phase before menopause is called the perimenopause and the phase after menopause is called postmenopause.
This phase starts several years before menopause. Here, the ovaries start producing less estrogen gradually through the time which is why you start getting your periods irregularly. You might notice that as time passes by, the gap in between your periods increases. Many may also start to experience the various menopausal symptoms like hot flashes that are sudden flares of heat and sweating, mood swings due to the hormone imbalances and vaginal dryness that leads to dry and irritated vulva. This phase is a transition to actual menopause and usually starts when you are in your 40s. As you are still having menstrual cycles during this time, you can still get pregnant.
Now as your periods continue being irregular, menopause is when the occurrence of periods completely stops. Your estrogen levels have been dropped to a significant level and your menstrual cycle has completely ceased. Officially, menopause is declared after 12 consecutive months without a menstrual period. Again, the symptoms of menopause continue to persist. On an average, menopause happens from ages 51-55.
This is the phase after menopause that lasts for the rest of a woman’s life. This is where the estrogen levels have stabilized at a lower level and you might not experience most of the menopausal symptoms anymore. However, due to the low estrogen levels, postmenopausal women are more vulnerable to various health conditions like heart diseases and osteoporosis.
Before menopause, estrogen provides some protection against heart disease by helping to keep arteries flexible and promoting healthy levels of cholesterol. After menopause, when estrogen levels decline, this protective effect diminishes, hence leading to an increased risk of heart disease. To deal with it, it is important for women to maintain a healthy weight and opt for a diet low in saturated fats and cholesterol.
Estrogen plays a crucial role in maintaining bone density too. After menopause, the declining estrogen can lead to rapid bone loss and an increased risk of osteoporosis which results in weakened, brittle bones that are more susceptible to fractures. Hence it is important to intake calcium and vitamin D through diet or supplements.
Menopause is a journey that every woman has to go through in her life. Understanding what actually happens inside the body makes it easier for us to manage it. Getting educated about the various issues that one might face, gives us plenty of time to prepare for it and take lifestyle and treatment approaches that are suitable.

Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder affecting millions of women worldwide. Characterized by irregular periods, ovarian cysts and hormonal imbalances, PCOS can impact various aspects of a woman’s health and well-being. PCOS is often associated with insulin resistance, which can lead to weight gain, difficulty losing weight and an increased risk of Type 2 diabetes. Hormonal imbalances, including elevated levels of androgens (male hormones), can cause acne, excessive hair growth and hair loss of the scalp. PCOS is a leading cause of infertility due to irregular ovulation. While there’s no cure for PCOS, adopting a healthy lifestyle helps to manage the condition.
Firstly it is very important to pay attention to the foods you consume. Opting for food that are nutrient-dense and whole foods like fruits, vegetables and lean proteins help in contributing to a healthier lifestyle while incorporating anti-inflammatory foods like fatty fish, nuts, seeds and leafy greens helps to reduce inflammation associated with PCOS. Further try to limit refined carbohydrates and sugars, which can spike insulin levels and exacerbate PCOS symptoms.
Exercise plays an important role in managing the weight gained due to PCOS. Not just that, but movement helps to make sure that insulin sensitivity is improved and stress levels are reduced, which all are beneficial for PCOS management. Try to incorporate as much as cardiovascular exercises, strength training and flexibility exercises into your routine. Find activities you enjoy, whether it’s dancing, swimming, any physical sport or yoga to make exercise a sustainable part of your routine.
Prioritize quality sleep by establishing a consistent sleep schedule and creating a relaxing bedtime routine. Aim for 7-9 hours of sleep per night to support hormone regulation. Minimize exposure to screens and stimulating activities before bedtime to promote better sleep quality.
Chronic stress can exacerbate PCOS symptoms by increasing cortisol levels and disrupting hormonal balance. Incorporating stress management techniques into your daily routine can help reduce stress. Practice mindfulness meditation, deep breathing exercises or yoga to reduce stress levels and promote relaxation. Engage in activities that bring you joy and fulfillment, whether it’s spending time in nature, pursuing creative hobbies or connecting with loved ones. Prioritize self-care activities to nurture your physical and emotional well-being.
Lastly, consult your gynecologist regularly to stay updated on your progress in battling PCOS. Try to reach out to multiple women through online communities to share experiences and find encouragement from others facing similar challenges. Remember that small changes can lead to significant improvements over time so be patient and compassionate with yourself as you navigate your PCOS journey.

Premature Ejaculation is one of the most prevalent sexual disorders affecting men and yet is often surrounded by silence and stigma. Men may feel embarrassed or ashamed to talk about it and have an open discussion with their partners or doctors. However it is important to break this silence and recognize that premature ejaculation deserves attention and support. Men should gain a better understanding of the condition so they can learn about the various strategies for managing it.
Premature Ejaculation is a common sexual dysfunction marked by an inability to delay ejaculation during sexual intercourse, resulting in an orgasm that occurs sooner than desired by either partner. The exact cause is not fully understood but it is believed to involve psychological and biological factors. Psychological factors like anxiety, stress or past sexual experiences and biological factors like hormonal imbalances can contribute to Premature Ejaculation.
Now, the way to go at it depends on whether you have had this condition since the first sexual encounter or has it developed recently. If you have had this condition consistently over time, that indicates that you may have Lifelong (or primary) PE, but in case of the latter, you may have Acquired (or secondary) PE which is often associated with stress, relationship issues or performance anxiety. You can avoid Premature Ejaculation by building your Stamina and Endurance by engaging in regular cardiovascular and strength training activities. Strengthening your pelvic floor muscles with kegel exercises can help improve control during sexual activity. Apart from this, ensuring that you are getting adequate sleep, managing stress efficiently, limiting alcohol and smoking and drinking plenty of water is also important. You can consult a healthcare professional or a sex therapist for personalized advice and support.
Here are some common medications that your healthcare provider shall prescribe you but make sure that any medication you use should only be used under the guidance of a HCP as not all medications can be effective for some people and may come with potential side effects or interactions with other medications. SSRIs, that is Selective Serotonin Reuptake Inhibitors and TCAs, that is Tricyclic Antidepressants are classes of antidepressants that can help to delay ejaculation. Topical Creams containing anesthetics like lidocaine can also help to reduce sensitivity and delay ejaculation. Apart from that PDE5 Inhibitors like Viagra, which are commonly used to treat erectile dysfunction may also have some benefits in delaying ejaculation.
As medicated options for PE might pose certain risks and potential side effects, many feel safer going with natural remedies instead as they offer a gentler approach while potentially providing additional health benefits. Certain herbal supplements like Tribulus Terrestris, Ginseng, L-Arginine, Zinc and many more can have a positive effect on ejaculatory control. Try finding herbal or nutraceutical products that contain all these ingredients.

Navigating life as a young woman comes with its own set of challenges, from academic pursuits to career aspirations and personal growth. However, for many young women, another hurdle presents itself early on: Polycystic Ovary Syndrome (PCOS). PCOS is a hormonal disorder that affects millions of women worldwide, often manifesting during adolescence or early adulthood. From irregular periods to acne and weight gain, PCOS can significantly impact physical health and emotional well-being. Coping with PCOS at a young age requires patience and a proactive approach to self-care.
First and foremost, understanding PCOS is crucial. Educate yourself about the condition – its causes, symptoms, and potential complications. Knowledge empowers you to make informed decisions about your health and treatment options. PCOS research is continually evolving with new findings shaping treatment approaches and lifestyle recommendations. Stay updated on the latest developments by following reputable medical websites. Don’t hesitate to ask your healthcare provider questions about PCOS during appointments about the treatment options and how the condition affects various aspects of your life. Understanding the intricacies of the condition, its causes and symptoms empowers you to make informed decisions about your health.
Managing PCOS is not just about alleviating immediate symptoms, it’s also about prioritizing long-term health. Adopting healthy lifestyle habits like maintaining a balanced diet, regular exercise routine, adequate sleep and stress management practices can have a profound impact on managing PCOS symptoms and reducing long-term health risks. Schedule regular check-ups with your healthcare provider to monitor your PCOS and address any changes or concerns promptly.
Living with PCOS can feel isolating, but you’re not alone. Seek support from friends, family or even online communities of women facing similar challenges. Joining online forums or social media groups dedicated to PCOS can connect you with others facing similar experiences. These communities offer a platform to share stories and exchange advice. PCOS can impact mental health, leading to feelings of anxiety, depression or low self-esteem. Seeking therapy or counseling can also help you develop coping strategies and process emotions.

PCOS is a hormonal disorder causing enlarged ovaries with small cysts on the outer edges. Despite its prevalence, PCOS remains widely misunderstood leading to delayed diagnosis and management. Recognizing the signs of PCOS is the first step toward diagnosis and treatment. While symptoms can vary widely among individuals, common indicators of PCOS include:
Menstrual cycles may be irregular, with longer gaps between periods or unpredictable bleeding patterns.
Excessive hair growth in areas such as the face, chest or back often resembling male-pattern hair growth.
Persistent acne, particularly along the jawline, chin and cheeks is a common symptom of PCOS due to increased androgen levels.
Difficulty losing weight or unexplained weight gain, often concentrated around the abdomen is prevalent among individuals with PCOS.
Thinning hair or male-pattern baldness known as alopecia can occur in women with PCOS due to hormonal imbalances.
Skin changes such as darkening or thickening of the skin in body folds like neck creases, groin and under the breasts may indicate insulin resistance.
If you’re experiencing the following symptoms suggestive of PCOS, it’s essential to consult a healthcare provider for evaluation and diagnosis. Detecting Polycystic Ovary Syndrome (PCOS) at an early age allows for prompt intervention to manage symptoms and avoid potential complications effectively. Early intervention may include lifestyle modifications, hormonal therapy or medications to regulate menstrual cycles, control acne and manage weight. PCOS is associated with various long-term health risks including type 2 diabetes, cardiovascular disease and endometrial cancer. Detecting PCOS early provides an opportunity to implement preventive measures and to reduce the risk of developing these conditions later in life. For example, early intervention to address insulin resistance can help prevent the onset of diabetes and cardiovascular complications associated with PCOS.

Nowadays there are many many factors that contribute to declining reproductive health for men. It could be due to age, obesity, poor diet, lack of exercise, excessive alcohol consumption, medical conditions, and the list can go on and on. Having a proper diet that contains all the nutrients you require to ensure an optimal reproductive health is crucial to overall wellbeing. It also helps to keep yourself and your partner sexually satisfied. While it might be challenging to try to incorporate all of these ingredients in your diet on a daily basis, you can easily find these ingredients in nutraceutical formulations. By consuming the recommended dosage, you are making sure that your daily requirements for reproductive health are met.
Zinc – Zinc helps in the production of testosterone (the male reproductive hormone) and also improves sperm quality. It is scientifically proven to be helpful in increasing libido as well as in conditions like erectile dysfunction.
L-Arginine – L-Arginine helps to improve blood flow to the genitals, enhancing erectile function. It also tackles conditions like premature ejaculation and improves libido and virility.
Coenzyme Q10 – It is an antioxidant that supports sperm health and motility. It helps in improving the sperm count, sperm concentrations and sperm morphology.
Tribulus terrestris – Tribulus terrestris enhances libido and improves erectile dysfunction by increasing testosterone levels.
Omega -3 fatty acids – Omega 3 fatty acids can particularly help to improve sperm quality and motility.
These ingredients ensure that your reproductive health stays at peak but also boosts libido and enhances sexual performance which can also help to improve your relationships. As these ingredients are completely natural, you don’t have to worry about any side effects that one might often expect with medicated drugs.

Male infertility is a common concern that affects countless couples worldwide. However, advancements in science and medicine have led to the development of innovative solutions to address this issue. One such breakthrough is GinSperm, a unique formulation containing Korean Red N-216, a potent ingredient that has shown promising results in improving male fertility. In this blog, we will delve into the benefits of GinSperm and explore how its key ingredient, Korean Red N-216, enhances sperm count, quality, hormonal balance, and overall reproductive health.
GinSperm stands out due to its inclusion of Korean Red N-216, a powerful ingredient that offers significant benefits for male fertility. Korean Red N-216 is a cyclic adenosine monophosphate-responsive element modulator, which means it plays a crucial role in regulating gene expression related to male reproductive health. This unique compound has been scientifically studied and has shown promising results in improving fertility parameters in men.
GinSperm, fortified with Korean Red N-216, effectively improves key aspects of sperm health. It enhances sperm count, which is essential for increasing the chances of successful conception. Additionally, it improves sperm motility, ensuring that sperm can move effectively towards the egg. Moreover, GinSperm promotes optimal sperm morphology, enhancing the shape and structure of sperm, which is crucial for successful fertilization.
Testosterone, the primary male sex hormone, plays a vital role in sperm production. GinSperm, with its key ingredient Korean Red N-216, increases testosterone levels and enhances androgen receptor activity. This combination promotes healthy sperm production, ensuring a higher quantity of quality sperm, and improving overall fertility.
Stress and anxiety can negatively impact male fertility by disrupting hormone balance. GinSperm addresses this concern by reducing stress and anxiety levels. By balancing hormone status, it creates a favorable environment for optimal reproductive function and increases the chances of successful conception.
Erectile dysfunction can be a contributing factor to male infertility. GinSperm supports erectile function by increasing nitric oxide production, a compound that helps relax blood vessels and improves blood flow to the reproductive organs. Furthermore, GinSperm reduces oxidative stress, a common cause of sperm damage, thereby improving overall sperm health and fertility. By supporting overall health and well-being, GinSperm enhances the chances of successful conception.
GinSperm not only targets sperm health but also supports the overall health of reproductive organs. By improving blood circulation to these organs and reducing inflammation, it creates an optimal environment for reproductive function. Additionally, GinSperm supports the immune system, ensuring the body’s defense mechanisms are functioning optimally, which is vital for maintaining reproductive health.
Male infertility can be a challenging obstacle on the path to parenthood, but with advancements in science and innovative formulations like GinSperm, hope is within reach. GinSperm, with its unique ingredient Korean Red N-216, offers a holistic approach to improving male fertility. By enhancing sperm count, quality, testosterone levels, and overall reproductive health, GinSperm empowers men on their journey to fatherhood. With its ability to reduce stress, improve erectile function, and support the immune system, GinSperm goes beyond addressing fertility concerns and promotes overall well-being. Consider adding GinSperm to your fertility regimen and embark on the path to enhanced male fertility and the dream of starting or expanding your family.

Erectile dysfunction (ED) is basically the inability of a man to achieve or maintain an errection that is sufficient for sexual satisfaction. It happens due to several underlying factors that could be linked to physical or even emotional wellbeing. Erection occurs when nerves signal the blood vessels in the genitals to relax and widen leading to an increased blood flow that causes the organ to become erect. Regardless, it can create challenges in relationships with your partner.
Erectile Dysfunction can lead to a man feeling embarrassed about himself and hence withdrawing from communicating openly as well. This frustration and tension can strain the relationship. Intimacy is not just about the sexual activity, however ED can also impact affection between partners which brings down the overall intimacy as well.
Erectile Dysfunction can greatly affect a man’s self-esteem and confidence which in turn influences their behaviour. If it is not addressed properly, it can also lead to mental health issues like depression or anxiety.
All these are ways in which the man in the relationship can get affected, but due to the feelings of sexual insatisfaction, there may be negative emotions of disappointment and resentment from both the partners. These emotions tend to create tension and distance in the relationship.
Open communication is the key when it comes to managing Erectile Dysfunction. A man should not be embarrassed to talk about it with his partner and the woman should also be understanding enough about the situation. It requires effort and patience. You can also seek for advice from a doctor if the condition is persistent.
Additionally, there are multiple natural ingredients that are scientifically proven to address Erectile Dysfunction and help achieve sexual satisfaction in the bedroom. Look out for ingredients like Tribulus terrestris, Zinc, L-Arginine in natural formulations.

Infertility is often considered a topic mainly associated with women when they struggle to get pregnant. However, it’s essential to recognize that men can also face fertility challenges. Male infertility affects millions of couples worldwide, yet it is often shrouded in silence and stigma. There shouldn’t be a differentiation in men and women with respect to the emotional aspect. In this blog, we aim to shed light on the stigma surrounding male infertility, explore its impact on men and their partners, and discuss ways to empower men in overcoming this stigma. By being understanding and supportive, we can create a more inclusive and compassionate environment for those affected by male infertility.
The first step in differentiating the stigma of male infertility is to break the silence surrounding the topic. Traditionally, societal expectations have placed the burden of becoming pregnant on women, leading to a lack of awareness and support for men facing fertility challenges. Men, too, may feel societal pressure to conform to traditional gender roles, which can make it difficult for them to open up about their struggles with infertility. By encouraging open conversations, we can create a safe space for men to share their experiences without the fear of judgment or shame.
Stereotypes associated with male fertility can further perpetuate the stigma surrounding male infertility. Society often equates masculinity with fertility, creating an environment where men who experience fertility challenges may feel emasculated. It is crucial to differentiate these stereotypes and redefine what it means to be a man. Fertility struggles do not diminish a man’s worth or masculinity. By promoting a more inclusive and understanding definition of masculinity, we can combat the stigma and empower men to seek help and support.
Educating both men and society at large about male infertility is vital in overcoming the stigma. Many people lack accurate information about the causes, prevalence, and treatments available for male infertility. By providing comprehensive and accessible education, we can avoid myths and misconceptions among people. Support groups, counseling services, and online communities can play a crucial role in connecting men and their partners with others who share similar experiences. These platforms provide a safe space to share stories, seek advice, and offer support, helping individuals navigate their fertility journey with greater confidence and resilience.
The impact of male infertility extends beyond the individual, affecting the couple as a whole. It is essential to involve partners in discussions and decision-making processes, fostering a sense of shared responsibility and support. Open and honest communication within the relationship can help build trust, strengthen emotional bonds, and navigate the challenges of infertility together. By acknowledging the shared experience and actively involving partners, we can reduce feelings of isolation and empower couples to face male infertility as a united front.
Differentiation of the stigma of male infertility requires collective efforts to foster understanding, empathy, and support. By breaking the silence, challenging stereotypes, providing education, and promoting partner inclusion, we can empower men and couples affected by male infertility. Let us create a world where individuals facing fertility challenges are met with compassion, where their voices are heard, and where they are empowered to seek the help they need to fulfill their dreams of getting pregnant.

Erectile dysfunction (ED) is basically the inability of a man to achieve or maintain an errection that is sufficient for sexual satisfaction. It happens due to several underlying factors that could be linked to physical or even emotional wellbeing. Erection occurs when nerves signal the blood vessels in the genitals to relax and widen leading to an increased blood flow that causes the organ to become erect. Regardless, it can create challenges in relationships with your partner.
Erectile Dysfunction can lead to a man feeling embarrassed about himself and hence withdrawing from communicating openly as well. This frustration and tension can strain the relationship. Intimacy is not just about the sexual activity, however ED can also impact affection between partners which brings down the overall intimacy as well.
Erectile Dysfunction can greatly affect a man’s self-esteem and confidence which in turn influences their behaviour. If it is not addressed properly, it can also lead to mental health issues like depression or anxiety.
All these are ways in which the man in the relationship can get affected, but due to the feelings of sexual insatisfaction, there may be negative emotions of disappointment and resentment from both the partners. These emotions tend to create tension and distance in the relationship.
Open communication is the key when it comes to managing Erectile Dysfunction. A man should not be embarrassed to talk about it with his partner and the woman should also be understanding enough about the situation. It requires effort and patience. You can also seek for advice from a doctor if the condition is persistent.
Additionally, there are multiple natural ingredients that are scientifically proven to address Erectile Dysfunction and help achieve sexual satisfaction in the bedroom. Look out for ingredients like Tribulus terrestris, Zinc, L-Arginine in natural formulations.

Nowadays there are many many factors that contribute to declining reproductive health for men. It could be due to age, obesity, poor diet, lack of exercise, excessive alcohol consumption, medical conditions, and the list can go on and on. Having a proper diet that contains all the nutrients you require to ensure an optimal reproductive health is crucial to overall wellbeing. It also helps to keep yourself and your partner sexually satisfied. While it might be challenging to try to incorporate all of these ingredients in your diet on a daily basis, you can easily find these ingredients in nutraceutical formulations. By consuming the recommended dosage, you are making sure that your daily requirements for reproductive health are met.
Zinc – Zinc helps in the production of testosterone (the male reproductive hormone) and also improves sperm quality. It is scientifically proven to be helpful in increasing libido as well as in conditions like erectile dysfunction.
L-Arginine – L-Arginine helps to improve blood flow to the genitals, enhancing erectile function. It also tackles conditions like premature ejaculation and improves libido and virility.
Coenzyme Q10 – It is an antioxidant that supports sperm health and motility. It helps in improving the sperm count, sperm concentrations and sperm morphology.
Tribulus terrestris – Tribulus terrestris enhances libido and improves erectile dysfunction by increasing testosterone levels.
Omega-3 fatty acids – Omega 3 fatty acids can particularly help to improve sperm quality and motility.
These ingredients ensure that your reproductive health stays at peak but also boosts libido and enhances sexual performance which can also help to improve your relationships. As these ingredients are completely natural, you don’t have to worry about any side effects that one might often expect with medicated drugs.

When we think about infertility, the conversation often revolves around women and their reproductive health. However, it is essential to shed light on the silent struggle faced by men—male infertility. In this blog, we will explore the various aspects of male infertility, including its causes, effects, and the importance of raising awareness about this often-overlooked issue.
Male infertility refers to the inability of a man to contribute to a successful pregnancy after a year of regular, unprotected intercourse. It is a widespread concern, affecting millions of couples worldwide. In fact, male infertility contributes to nearly 40-50% of all infertility cases.
Lets first understand the structure and function of the sperm. A sperm cell has a unique structure that is tailored for its specific function. It consists of three main parts – head, midpiece and tail (flagellum). The primary function of sperm is to fertilize the female egg. The nucleus of the sperm carries the genetic material in the form of DNA. It contains the instructions necessary for the development and functioning of an organism. During fertilization, the sperm’s nucleus fuses with the egg’s nucleus, combining the genetic material from both parents to create a new individual with a unique set of genes. The mitochondria, located in the midpiece of the sperm, provide the energy required for sperm motility and other cellular processes. They generate ATP (adenosine triphosphate), which serves as the energy currency of the cell. The mitochondria play a crucial role in powering the sperm’s swimming motion, allowing it to reach the egg.
Despite its prevalence and significant impact, male infertility often remains a silent struggle due to societal expectations and misconceptions. Men may hesitate to seek help or share their experiences due to fear of judgment or societal pressures.
Raising awareness about male infertility is crucial for breaking the silence and fostering a supportive environment. By encouraging open conversations, we can reduce stigma, provide a platform for individuals to share their stories, and offer support and understanding to those facing male infertility.
The first step in addressing male infertility is seeking professional help. A healthcare provider specializing in fertility can perform comprehensive evaluations and diagnostic tests to identify the underlying causes. These tests may include semen analysis, hormone testing, genetic screenings, and imaging studies.
Male infertility is a common but often overlooked issue that impacts individuals and couples worldwide. By understanding its causes, effects, and the importance of raising awareness, we can create a supportive environment for those facing this silent struggle. It is crucial to break the silence, encourage open conversations, and seek professional help when needed. With the right support and available treatments, individuals and couples can navigate the challenges of male infertility and find hope on their path to parenthood.
Multiple times we have heard that alcohol is bad. That it negatively impacts your liver. Not just your liver but it also contributes to cardiovascular problems like hypertension, heart disease and stroke, gastritis, pancreatitis, digestive problems, mental health disorders like depression and anxiety as well as overall energy levels affecting daily functioning. Let us understand how exactly it impacts our liver especially when consumed in high levels on a regular basis.
Alcohol contains ethanol which is directly toxic for the cells in the body especially affecting the central nervous system. Chronic exposure to long levels of ethanol can lead to neurotoxicity and cognitive deficits. The metabolism of alcohol also promotes oxidative stress which contributes to tissue inflammation and organ damage.
The first metabolite of ethanol – Acetaldehyde is highly toxic. It can cause damage to cells and tissues, particularly in the liver where it contributes to inflammation and oxidative stress. Acetaldehyde is also carcinogenic and has been implicated in the development of cancers including liver cancer (hepatocellular carcinoma).
Our liver is continuously synthesizing proteins that are essential for maintaining the structure and function of liver cells as well as proteins that are involved in various metabolic processes. Chronic alcoholic consumption disrupts the liver’s ability to synthesize these proteins. The proteins involved in detoxification pathways that breaks down and removes toxins from our body get particularly affected.
Enzymes that help convert alcohol to less toxic substances are also affected. Regular long term alcohol consumption can alter the activity of these enzymes leading to a buildup of toxic metabolites.
As the liver plays an important role in metabolism of other nutrients like carbohydrates, fats and various proteins, alcohol can also impair the liver’s ability to carry out essential metabolic functions.
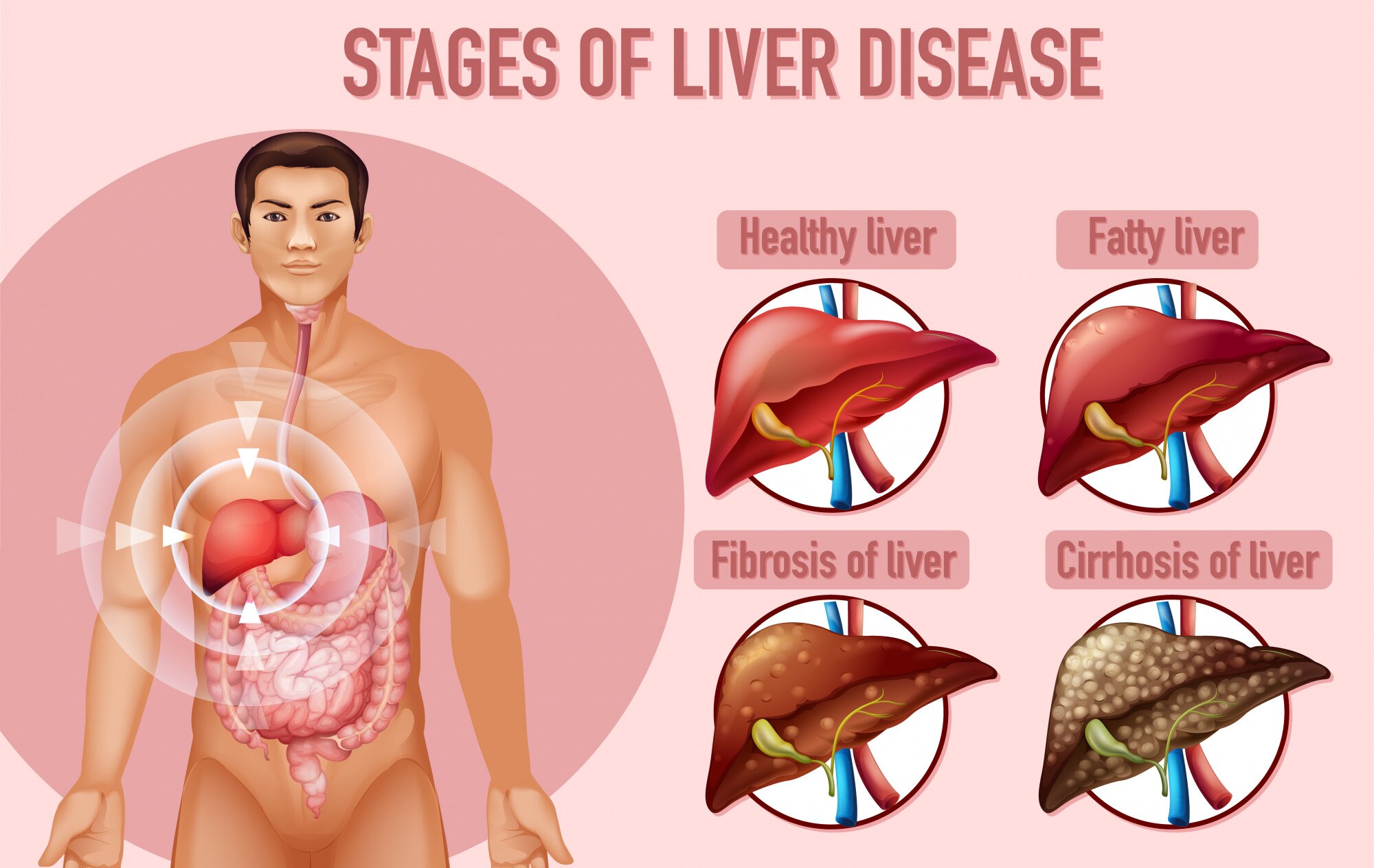
Fatty Liver – Alcohol metabolism primarily occurs in the live and this process can lead to an imbalance in the liver’s normal fat metabolism, resulting in the accumulation of fat within liver cells. This condition is known as fatty liver or steatosis. Fatty liver is often reversible if alcohol consumption is stopped early.
Alcoholic Hepatitis – Prolonged and excessive alcohol consumption can lead to inflammation of the liver known as alcoholic hepatitis. This inflammation occurs due to the toxic effects of acetaldehyde, oxidative stress from alcohol metabolism and the body’s immune response to damaged liver cells. Continued alcohol use exacerbates this condition and increases the risk of progressing to more severe liver damage.
Fibrosis – Fibrosis is the formation of scar tissue in the liver. Over time as fibrosis progresses, it can impair liver function and lead to other complications
Cirrhosis – Cirrhosis is the advanced stage of liver fibrosis where extensive scar tissue replaces healthy liver tissue. Cirrhosis is irreversible and severely impairs liver function.Cirrhosis is a major risk factor for liver cancer.
Our kidneys are vital organs that play a crucial role in maintaining our overall health. They filter waste and excess fluids from the blood, regulate blood pressure and help control electrolyte balance. However, kidneys are susceptible to various diseases that can compromise their function. In this blog, we will explore some common types of kidney problems, their causes, symptoms and potential treatments.
Chronic Kidney Disease is a long-term condition where the kidneys gradually lose their ability to function properly. It is usually caused by underlying health conditions like high blood pressure and diabetes. Chronic Kidney Disease progresses in stages and in advanced stages, patients may require dialysis or kidney transplantation to survive. Early detection through regular check-ups is crucial to slow down its progression with the help of medications like dapagliflozin.
Acute Kidney Injury is a sudden and severe decline in kidney function often occurring as a result of a specific injury or medical condition. Causes of Acute Kidney Injury can include infections, severe dehydration, medication side effects or surgeries. Timely medical intervention is essential to reverse Acute Kidney Injury and prevent further damage.
Polycystic Kidney Disease is a genetic disorder characterized by the growth of fluid-filled cysts within the kidneys. These cysts can gradually enlarge, impairing kidney function and leading to complications such as high blood pressure and kidney stones. Treatment focuses on managing symptoms and complications as there is currently no cure for Polycystic Kidney Disease.
Kidney stones are solid mineral deposits that form in the kidneys often causing severe pain when they move through the urinary tract. They can result from factors like dehydration, diet and genetics. Treatment may involve pain management, lifestyle changes or medical procedures to remove or break down the stones.
Glomerulonephritis is a group of diseases that damage the glomeruli, tiny filters in the kidneys responsible for removing waste and excess fluids from the blood. Inflammation in the glomeruli can result from infections, autoimmune disorders or other underlying conditions. Management may include medications to reduce inflammation and treat the underlying cause.
UTIs are bacterial infections that can affect any part of the urinary system including the kidneys. Symptoms may include pain, frequent urination and fever. Timely treatment with antibiotics is crucial to prevent the spread of infection to the kidneys which can lead to more severe complications.
Kidney diseases can have a profound impact on an individual’s health and well-being. Early detection, lifestyle modifications and appropriate medical management are essential in preventing and managing kidney-related issues. Regular check-ups with a healthcare provider, maintaining a healthy diet, staying hydrated and managing underlying conditions like diabetes and high blood pressure can go a long way in preserving kidney function and overall health. If you experience any kidney-related symptoms it’s essential to seek medical attention promptly to address the issue before it progresses.

Pyelonephritis is a potentially serious kidney infection that can occur when a urinary tract infection (UTI) typically cystitis (bladder infection) progresses into the kidneys. This condition can lead to various complications including sepsis and osteomyelitis. In this blog, we’ll explore what pyelonephritis is, its causes, symptoms and the relationship between pyelonephritis, sepsis and osteomyelitis.
Pyelonephritis is an infection that affects the upper urinary tract primarily the kidneys. It typically arises from bacteria traveling up the urethra and into the bladder causing cystitis (bladder infection). If left untreated or inadequately managed, the bacteria can ascend further into the ureters and reach the kidneys leading to pyelonephritis.
The most common cause of pyelonephritis is the migration of bacteria such as Escherichia coli (E. coli) from the lower urinary tract into the kidneys. Factors like urinary tract obstructions, pregnancy or weakened immune systems can increase the risk of this bacterial invasion. When cystitis/ bladder infection is not treated promptly, the bacteria can multiply and spread eventually reaching the kidneys and causing pyelonephritis.
Symptoms of pyelonephritis include high fever, flank pain, frequent and painful urination, cloudy or bloody urine, nausea, vomiting and fatigue.
Sepsis is a severe and potentially life-threatening condition that can result from pyelonephritis. When the infection spreads to the bloodstream, it triggers a systemic inflammatory response leading to sepsis. Symptoms of sepsis include a high fever, rapid heart rate, confusion and organ dysfunction. Immediate medical attention is crucial to treat sepsis.
Osteomyelitis is a rare but possible complication of pyelonephritis. It occurs when the infection spreads to the bones often affecting the vertebrae in the spine. Symptoms of osteomyelitis include localized pain, swelling, and fever. Timely diagnosis and appropriate treatment which may involve antibiotics and surgical intervention are essential to manage this condition.
Early intervention is crucial in preventing the progression of urinary tract infections (UTIs) to pyelonephritis, a potentially serious kidney infection. Timely treatment with antibiotics is the primary approach to address pyelonephritis effectively. Moreover, adopting proactive measures such as staying well-hydrated and practicing good hygiene can significantly reduce the risk of developing UTIs, thus contributing to the prevention of pyelonephritis.
Recognizing the symptoms of pyelonephritis and seeking prompt medical attention is crucial to prevent adverse kidney problems. Additionally, practicing good urinary tract health, staying hydrated and addressing UTIs promptly are essential steps in reducing the risk of pyelonephritis and its associated complications. If you suspect you may have a UTI or are experiencing symptoms of pyelonephritis, consult a healthcare professional for proper evaluation and treatment.
The liver is a remarkable organ known for its regenerative capabilities. It has the unique ability to repair and regenerate damaged tissue which enables it to recover from a wide range of injuries and insults. While the liver is indeed a regenerative organ with a remarkable capacity for self-repair, certain liver diseases can have detrimental effects on the kidney’s problems. It’s essential to monitor and manage liver diseases carefully as their progression can lead to kidney problems.
The liver and kidneys are both involved in filtering and detoxifying the blood. The liver processes and metabolizes toxins, drugs and metabolic waste products from the bloodstream, converting many of them into water-soluble compounds that can be excreted by the kidneys. This collaboration helps eliminate waste and maintain the body’s internal environment.
The liver produces urea, a waste product of protein metabolism which is eventually excreted by the kidneys in the form of urine. This process helps regulate nitrogen balance in the body.
Both organs play a role in regulating blood pressure. The liver helps regulate blood volume by producing proteins like albumin, which maintains oncotic pressure. The kidneys regulate blood pressure by controlling the volume of blood and the balance of electrolytes and hormones such as renin and aldosterone.
Hepatorenal syndrome (HRS) is a potentially life-threatening condition in which liver dysfunction often associated with advanced liver disease (cirrhosis) leads to kidney diseases and dysfunction. As liver function declines, it can cause changes in blood flow to the kidneys, leading to a reduction in normal kidney function and the development of HRS.
When the liver is damaged or unable to detoxify the blood effectively, toxins and waste products can build up in the bloodstream. These substances can place additional stress on the kidneys potentially leading to acute kidney injury (AKI) or worsening of existing kidney problems.
Liver diseases can result in fluid retention in the abdominal cavity known as ascites. The accumulation of excess fluid can increase pressure on the blood vessels and impair kidney function potentially leading to kidney diseases and dysfunction.
Liver diseases can disrupt the balance of electrolytes in the body such as sodium and potassium. These imbalances can affect normal kidney function and lead to complications like dehydration or electrolyte abnormalities.
Taking good care of your liver is really important for the health of your kidneys. Your liver is like a superhero that can fix itself when it gets hurt, but if it’s not working well because of various liver diseases, it can make your kidneys sick too. So it’s best to keep your liver healthy by seeing a doctor regularly, making healthy lifestyle choices and following any medical advice you get. This way, you’re not only helping your liver but also keeping your kidneys in good shape which is essential for your overall health.

Osteoporosis is a bone disease characterized by low bone density and deterioration of bone tissue, leading to an increased risk of fractures. It can also be very painful and cause a lot of discomfort. With the right approach, natural supplements can be valuable tools in the fight against osteoporosis and help individuals maintain strong and healthy bones across the spectrum of severity.
One such supplement is Mountain Korean Red Ginseng known for its potential to enhance bone mineral density and reduce the risk of fractures. This traditional herb contains bioactive compounds like ginsenosides – which have been shown to stimulate bone formation and promote stronger bones.
L-arginine is another natural supplement that holds promise for individuals with osteoporosis. It is an amino acid that is involved in various metabolic processes, including the production of nitric oxide which plays a crucial role in calcium absorption. By enhancing blood flow to the bones and promoting the synthesis of collagen, l-arginine can contribute to bone repair.
Magnesium is a vital mineral that is essential for bone health, as it is involved in bone formation and density regulation. Adequate magnesium intake is crucial for maintaining optimal bone strength and structure, as well as supporting overall musculoskeletal health. Supplementing with magnesium can help prevent bone loss and reduce the risk of fractures in individuals with osteoporosis.
Cyanocobalamin which is also known as vitamin B12 is another natural supplement that can benefit individuals with osteoporosis. Vitamin B12 plays an important role in bone mineralization and its deficiency has been linked to an increased risk of osteoporosis and bone fractures. Supplementing with cyanocobalamin can help maintain healthy bone density and reduce the risk of osteoporotic fractures.
Incorporating natural supplements into your osteoporosis management plan can complement conventional treatments and support overall bone health. You can opt for supplements which provide all these ingredients in a single dosage as well. However, it is essential to consult with a healthcare professional before starting any new supplement regimen, especially if you have underlying health conditions.